DIABETES & EYE EXAMS
DIABETES & EYE EXAMS
If you are lucky enough to have good eyesight, you may be surprised when your diabetes care team recommends that you make an appointment with an eye doctor. If your vision is stable, and your eyes don’t bother you, why should you have your eyes checked?
The answer is that many potentially devastating eye problems develop without causing discomfort or distorting vision. Glaucoma and cataract are examples of eye problems that occur commonly in older adults and more frequently in people with diabetes. Generally, these conditions are treatable, but if not caught early enough, they can lead to vision loss or even blindness.
DIABETIC RETINOPATHY
The main reason people with diabetes are encouraged to have regular eye exams is to look for changes in the blood vessels of the retina that indicate diabetic retinopathy. Diabetic retinopathy develops as prolonged exposure to high blood glucose weakens the walls of the blood vessels in the eyes. The longer a person has had diabetes and the greater his exposure to high blood glucose, the greater his risk of having this condition.
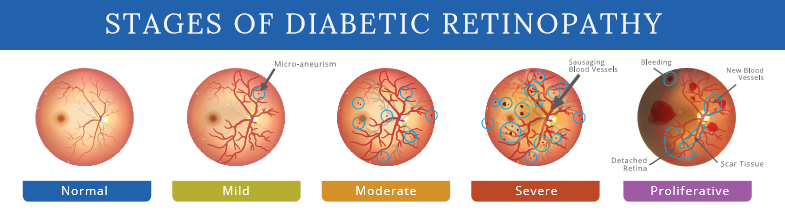
The earliest signs of diabetic retinopathy are little red or white spots on the retina that can only be seen by an eye doctor. These spots are microaneurysms, tiny pouches of blood that have bulged through the damaged blood vessel walls and can leak blood, fat, and fluid into the retinal tissues. These early changes in the blood vessels are called background, or nonproliferative, retinopathy. Leaking in the retina from background retinopathy can cause some blurring of vision, but it does not usually require immediate treatment.
If diabetic retinopathy causes damage near the macula, however, fluid leaking into the macula makes it swell like a mosquito bite. This swelling, called macular edema, is the most common cause of visual impairment in diabetic retinopathy. (Reduced blood supply to the macula is a less common occurrence. As yet, it is not treatable.)
The earliest changes of retinopathy can even be temporary: here today and gone in six months. If damage continues, though, the risk increases that new, abnormal blood vessels will start to sprout in retina and poke through into the vitreous. This important change is called going from background retinopathy to proliferative retinopathy.
The new blood vessels apparently proliferate in an attempt to increase blood and oxygen supply to the damaged retina. They are so fragile, though, that they rupture at a cough, a sneeze, or even during sleep. Blood pours into the retina, blocking vision suddenly. When the bleeding stops, scar tissue forms, tugging at the retina and adding the potential for a retinal detachment.
Untreated proliferative retinopathy usually leads to blindness. Not long ago, diabetic retinopathy was just about the most discouraging condition that ophthalmologists had to deal with. Fortunately, in recent years, a number of large national studies have proven that laser treatment of the retina can help control proliferative diabetic retinopathy and significantly prolong useful vision.
Ironically, laser treatment works by producing scarring on the affected retina. The treated part of the retina will no longer see, but the laser treatment halts the growth of new blood vessels and preserves vision in the most important part of the retina, the macula. Laser treatment for diabetic retinopathy is a tremendous tool that has expanded the ability to treat diabetic eye problems.
A surgical procedure called a vitrectomy, in which blood, scar tissue, and vitreous are removed from the eye and replaced with a saline solution, is also a relatively new, successful treatment for retinopathy that affects the vitreous. The medicines ranibizumab and aflibercept are also approved to treat diabetic retinopathy in people with diabetic macular edema.
LOOKING OUT FOR YOUR EYES
In a study published in the March 2001 issue of Diabetes Care researchers studying retinal photographs taken during the Diabetes Control and Complications Trial discovered that in people with Type 1 diabetes, the progression of diabetic retinopathy begins even earlier than had previously been thought. Waiting up to five years to have an initial eye exam is too long, they suggested, because it may already be too late for the best treatment. They concluded that all individuals newly diagnosed with Type 1 diabetes should have an eye exam upon diagnosis.
With recent improvements in treatments, the chances of avoiding vision loss from diabetes- and age-related eye conditions are greater than ever, but vigilance is key. If you have never had a dilated eye exam or haven’t had one within the past year, ask your doctor for a referral to an eye-care professional who is trained to diagnose diabetic retinopathy. Take this important step now, and follow up with yearly visits.
